MULTIPLE SCLEROSIS
Multiple Sclerosis Might be Triggered from a Leaky Blood-Brain Barrier
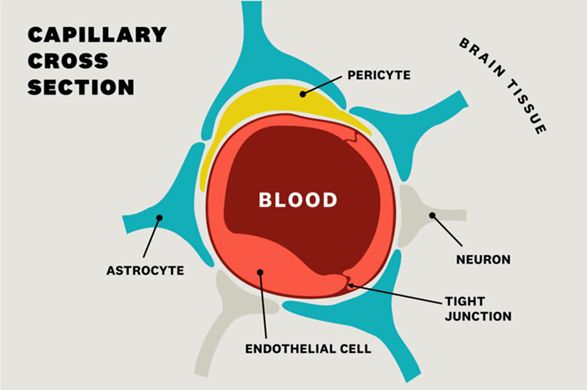
Multiple sclerosis (MS) has traditionally been viewed as an autoimmune disease in which the body attacks its own neurons. Recent hypotheses and evidence suggest that it might be caused by leaky blood vessels in the brain. The brain has a very strong blood-brain barrier that allows in oxygen and nutrients and the removal of wastes. Much attention has been focused on disruption of the blood-brain barrier. The blood-brain barrier is the very tight coupling of adjacent endothelial cells that line all of the small capillaries in the brain (Figure 1).
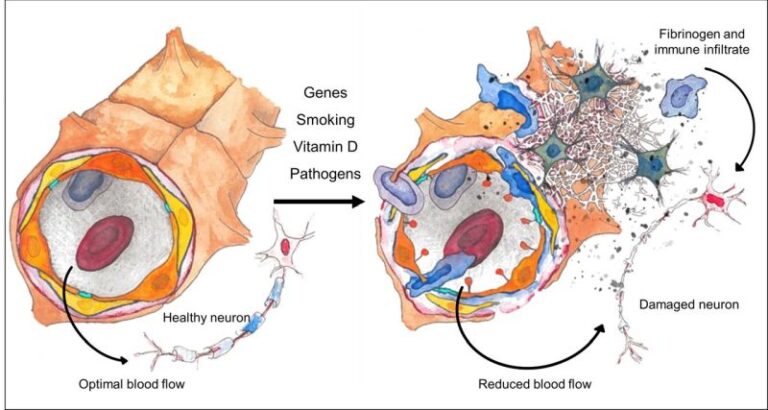
In multiple sclerosis, researchers now believe that a perfect storm of genetic and environmental factors can act together on the brain’s microvasculature and the blood-brain barrier resulting in a lack of nourishment to the neurons, as well increased blood-brain barrier permeability. This dysfunctional barrier leads to leakage which causes the immune cells to attack the central nervous system as shown in Figure 2.
On the left in Figure 2 is a healthy blood vessel which has optimal blood flow and healthy neurons. On the right is a damaged blood vessel with multiple insults which lead to disruption of the blood-brain barrier resulting in leakage of immune cells and toxic proteins (fibrinogen) which damage neurons in the vicinity.
As shown in Figure 2, optimal blood flow and an intact blood-brain barrier lead to healthy neurons in the central nervous system. Assault on the brain’s microvasculature by defective genes, smoking, Vitamin D deficiency, pathogens and aging leads to reduced cerebral/spinal cord blood flow and blood-brain barrier disruption, allowing the escape of attacking immune cells and the deposition of large and toxic proteins onto the nerve fibers (one such toxic protein is fibrinogen as shown on the right side of Figure 2).
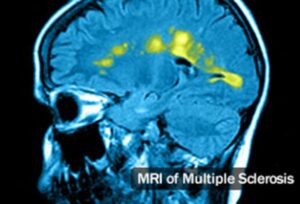
Reduced blood flow and disruption of the blood-brain barrier appear to interact in a vicious cycle, driving the destruction of neurons and the generation of focal lesions in the central nervous system which is the hallmark of MS pathology. In Figure 3 (source: WebMD.com), nuclear magnetic imaging displays the tell-tale focal lesions can be seen in the brain of a subject with MS.
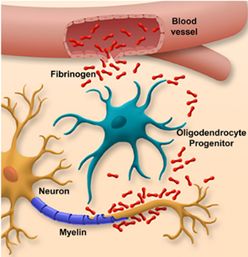
As stated above, disruption of the blood-brain barrier results in the leakage of large proteins out of the blood’s circulation into regions of the brain where they would not normally be located. One such protein, fibrinogen, is a large, “sticky” protein whose normal function within the blood vessel is to initiate the blood clotting. However, in MS where the blood-brain barrier has broken down, fibrinogen can now escape from the blood vessels and coats the neurons and the long axons that branch from the cell body of the neuron (Figure 4). This causes a toxic reaction as cells in the brain that normally patrol the brain (microglial cells) see this fibrinogen coated neuron as abnormal and attack it.
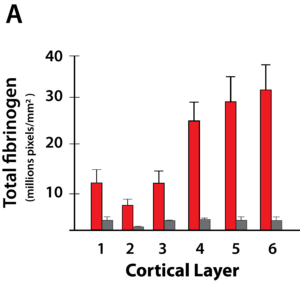
The red bars in the Figure 5 indicate fibrinogen levels in the cortex of MS patients. The gray bars are normal individuals. Figure 5 shows the incredibly high amount of fibrinogen that is seen in cortical layers of the brain in MS patients (red bars) when compared to normal individuals (gray bars). This huge deposition of toxic fibrinogen on cortical neurons would certainly contribute to the pathology seen in MS.
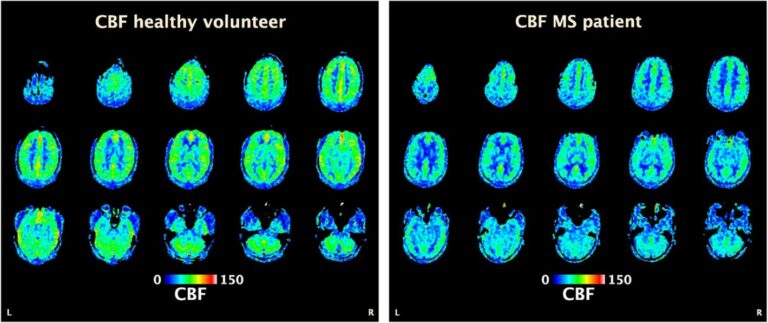
Another clinical finding that could suggest the development of ischemic brain lesions in individuals with MS is the observation that MS patients have globally decreased cerebral blood perfusion (CBF).
Studies using dynamic susceptibility contrast-enhanced MRI have demonstrated a globally decreased CBF, as compared to healthy patients. Overall, these findings suggest that reduced CBF is an early and integral feature of the disease, independent of its clinical course.
Brain perfusion is globally decreased in MS. Figure 6 shows perfusion-weighted brain MRI (arterial spin labelling) from a 35-year old healthy male volunteer (Figure 6, left) versus a 34-year old man with relapsing-remitting MS (Figure 6, right), with CBF color-coded map overlay (expressed as mL/100 g/min). Brain perfusion is globally reduced in the MS patients, as compared to the healthy volunteer.
Conclusion
It is well established that patients with MS also have other cardiovascular issues that point to a general dysfunction of the vascular system in this disease. Patients with MS have an increased risk for ischemic stroke and an increased risk of venous thrombosis and pulmonary embolism. Vascular comorbidities outside of the central nervous system are common in MS and can contribute to the disability seen in the disease. Evidence is mounting that vascular disease and endothelial cell dysfunction may be an important factor initiating and causing neuronal dysfunction and degeneration seen in multiple sclerosis.
Based on a large and accumulating body of evidence, it appears that vascular dysfunction and diminished blood flow in the brain, is an initiating factor in the development of neurodegenerative diseases, including multiple sclerosis. There is no single unifying theory of what causes MS, but there is very good medical evidence that blood-brain barrier disruption and vascular changes are a prominent and early feature of MS pathogenesis, which may be influenced by genetic and environmental risk factors for MS. These early vascular events could initiate a cascade of events which ultimately generates an immune response against the central nervous system and leads to MS.
Wund believes that focusing on the peripheral immune system alone, without taking in the contribution of the vascular system, may be limiting our understanding of the disease and the success of developing therapies for MS. A potent growth factor such as human FGF-1, which can stimulate the growth of new blood vessels and repair defective blood vessels by its direct action on the endothelial cells that line the blood vessel wall, makes FGF-1 a very attractive candidate to test in patients with MS.
Research papers and additional readings:
1. Multiple sclerosis as a vascular disease. Alireza Minagar, Wenche Jy, J. J. Jimenez & J. Steven Alexander. (2006) Neurological Research 28: 230-235. (Link: https://www.ncbi.nlm.nih.gov/pubmed/16687046 )
2. Vascular aspects of multiple sclerosis. Miguel D’haeseleer, Melissa Cambron, Ludo Vanopdenbosch, Jacques De Keyser. (2011) Lancet Neurology 657-666. https://www.ncbi.nlm.nih.gov/pubmed/21683931 )
3. Vascular pathology in multiple sclerosis: reframing pathogenesis around the blood-brain barrier. Jonathan Spencer, Jack Bell, Gabriele DeLuca. (2018) J Neurol Neurosurg Psychiatry 89:42–52. https://www.ncbi.nlm.nih.gov/pubmed/28860328 )
4. Emerging roles of endothelial cells in multiple sclerosis pathophysiology and therapy. A. Minagar , AH Maghzi , JC McGee, & JS. Alexander. (2012) Neurol Research Oct;34(8):738-45. https://www.ncbi.nlm.nih.gov/pubmed/22828184 )